
Everyone Loses
Lucas* regularly expressed frustration about his parents’ “nagging” him. Though he is a young adult, he lives out home and is mostly dependent on his parents for all essentials. He gave permission to involve his parents in treatment, which is ideal in many cases. It was frustrating for his compulsions to impair his life so much in the first place—embarrassment and shame only increased when it was called to his attention what he was not doing for the 100th time.
While Lucas suffered, so did his parents. It broke their heart to see his struggles, and their desperation for him to find freedom from OCD were commonly expressed in moments when they thought he was being lazy, taking their investment in his therapy for granted, or just wasn’t listening. It’s rarely that simple.
Getting on the Same Page
Whenever it is possible, it helps to get close support (parents, significant others) on board with what recovery entails. I recommend bringing a loved one into therapy about 90% of the time just for support, education, and environmental considerations for recovery.
Recovery from OCD is not only possible, but the treatments we have for OCD are some of the most beneficial of all mental health therapies. The disease can be so utterly encroaching on day-to-day life that full treatment often requires a fuller approach involving the family.
When I first invited the Thompsons into my office, they were slightly on guard. After all, who invites parents into therapy unless they’re in trouble, right? Isn’t it like going to the principal’s office?! I can gladly tell parents off-the-bat that OCD is not causally linked to parenting (check out a great intro training on OCD here).
It was such a joy to get on the same page and for each person to feel validated and appreciated. I can look at each person in the room and acknowledge their pain. There is no competition here—pain is pain. The first session with loved ones typically involves just an introduction with lots of validation and commonly tears and sighs of relief. Parents, like the Thompsons, feel at their wits’ end often. Children with OCD—including adults—often feel the full weight of their “hostage-taking” disorder but also their parents’ hopes, which in many cases are the same as theirs, such as:
- Become a fully functioning, contributing member of society
- Minimize suffering
- Better communication
- Be self-sufficient
- Enjoy life
- Function well in relationships
- Finish school
- Pursue meaningful work
When clients and loved ones grasp that it’s not only individual behaviors that the sufferer of OCD needs to change (e.g., learn to not compulse when getting intrusions), but there are many systemic accommodations that grow up around the person suffering.
Out of Love
Often unlike enabling behaviors in addictions, Family Accommodation (FA) is commonly done out of love and attempts to help through a difficult moment by taking on extra responsibility for the person. Enabling is somewhat the opposite where another person encourages or supports the pursuit of something known to be bad.
Compulsions by Proxy
Family Accommodation, in simple terms, is compulsions by proxy—they function as a temporary relief that keeps the person with OCD stuck. Yes, if the sufferer were perfect, they would simply say no to all their compulsion. But this is the real world, and we all need many supports to live life well. In fact, more accommodation in families predicts more severity and worse outcomes. Here’s the good news: both OCD and family accommodation are very treatable! Anyone who is willing to roll up their sleeves and grow can find benefits. It’s all about learning how OCD works and what helps to overcome its terrible grip.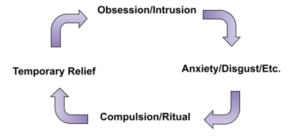 In the OCD Cycle above, instead of a client directly compulsing, accommodation is when the sufferer gets a “pass” from having to face the thing they need to do in order to get better. Maybe that is touching a door, not having Mom and Dad repeat something they just said until it’s “fully understood,” or it could be parents not giving reassurance that something is okay. There is nothing I can do that can replace that incredible sense of achievement that comes through doing exposures, tolerating uncertainty and doubt, and doing something that feels really scary but turns out okay.
In the OCD Cycle above, instead of a client directly compulsing, accommodation is when the sufferer gets a “pass” from having to face the thing they need to do in order to get better. Maybe that is touching a door, not having Mom and Dad repeat something they just said until it’s “fully understood,” or it could be parents not giving reassurance that something is okay. There is nothing I can do that can replace that incredible sense of achievement that comes through doing exposures, tolerating uncertainty and doubt, and doing something that feels really scary but turns out okay.
This is not a foreign concept. Imagine a child recovering from surgery and the doctor and physical therapist say it’s time to walk 1 mile per day and do stretches. The parent who does everything for the child, getting food from the fridge and pushing them in their wheelchair rather than letting them build strength is actually preventing them from getting better. Same concept.
Work Together for Full Recovery
When the Thompsons first came together, they were relieved and encouraged, but they also knew they had big steps ahead. The process is always “messy” to some extent. We need to keep communicating, stay flexible, and work on validating and loving even when feeling distressed or overwhelmed.
A Key Tip: Address Systemic AND Specific Accommodations
There are a lot of great further resources on this topic (see below to start), but one tip that I want to offer I haven’t seen discussed elsewhere is this: both systemic and specific accommodations need to be addressed for full benefit. Lucas thought after around session 9 that his parents weren’t accommodating him anymore. His parents believed the same. This is one reason to get a treatment specialist and/or someone objective on your team. What they were missing were the systemic accommodations.
Specific accommodations are more day-to-day:
- Buying more paper/cleaning products for the person with OCD than anyone else in the family
- Opening every door so they can avoid having to face it
- Doing the “dirty” cleaning for them, like toilets, bugs, or trash
Systemic accommodations are as the name implies, broader:
- Letting an adult child live in the house with no contribution
- Paying for everything
- Insulating a child from stress by handling things they need to do, such as making a phone call or filling out a form.
As you might imagine, addressing both of these are “sticky” areas and often require an expert to help. It can feel staggering to try to work on these things piecemeal, which is what a lot of families have tried for years and ended up in repetitive cycles of validation and understanding, accommodation, frustration, yelling, and hopelessness—to repeat it all again. There are a few ways to get started that I use in the office but don’t require therapy to learn more.
Take a Step Forward with These Free Tools
Bringing your challenges into the light is almost always the first step. Two ways I do this with clients:
-
- Family Accommodation Scale (FAS)—understand how much OCD is impacting everyone.
- Log (Track and Monitor)—identify what obsessions and compulsions are active. Both the person with OCD can use this form and a loved one’s observations to provide an outside perspective (though they might get some wrong, that’s okay!).
- Learn More—The Family Guide to Getting Over OCD: Reclaim Your Life and Help Your Loved One by Jonathan Abramowitz is the industry standard reference on family accommodation from one of the world’s foremost experts. Hear him on the OCD Stories podcast talking about this book and very detailed coverage of its contents. Also, did you know I have a free e-book on “Supporting Your Loved One With OCD”? Simply click on it to join a free list and get it immediately sent to your inbox along with several other resources.
*The key examples in stories I use are real, though I change the names and use composites of multiple people I have talked with and/or treated in a way that would make it impossible to identify them.







Leave a Reply