
What is CBT? Cognitive Behavioral Therapy is a mental health psychological treatment, or psychotherapy. The range of problems it treats is broad, from anxiety and depression to substance abuse and relationship problems. It is considered gold standard treatment (especially for OCD, Social Anxiety, and more). It is also seen as a first line treatment for a range of problems and goals. I’m here to help you nerd-out and understand a bit more about where it comes from and ideas on how it works.
Cognitive Behavioral Therapy in 3 Parts
CBT is often conceptualized on a triangle, such as the following “ABC”:
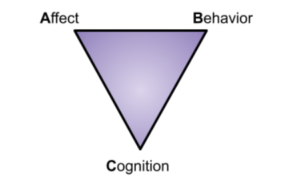
This triangle reflects no particular order or prioritization.
- A = Affect, or feelings and emotions
- B = Behavior, or actions
- C= Cognition, or thoughts and beliefs
CBT capitalizes on how each of these three domains have strong relationships to each other. The heart of the theory and practice is based on the knowledge that changing one or more of these domains leads to changes in the other. Another way of looking at it is that the more a person lines up their feelings, thoughts, and behaviors with reality, the more they achieve well-being, and many problems can be alleviated.
Every psychotherapy’s core question- and the role of theory.
By and large, it can be argued that any major system of psychotherapy at its heart is asking the question, “How does change occur in people? OR What effects change?” Change can be a quite comprehensive term, and may involve modification of feelings, distress, pain, suffering, hope, and much, much more. Many people don’t know that any medical treatment is born out of theory and still operates in the realm of various theories as to how and why they work. It is argued that the brain is the most complex object in the known universe, so staying “open-minded” (my attempt at a pun) and patient with learning is warranted. Even the assumption that mental health is brain health is based on, well, theory. And it may turn out to be overly reductionist from a research standpoint.
“All thinking involves theories….” (Alderson, 1998).
Most all my readers have experience with a traditional family doctor. They likely practice from what’s known as “the medical model,” which is a theoretical approach. Some may confuse this as only “symptom/problem focused,” but it is more pattern recognition (Aftab, 2020).
CBT is based out of both behavioral, social, and cognitive learning theories (Davis et al., 2017):
- Behavioral theories look at how external conditions impact behavior.
- Social learning indicates ways where learning can occur through observation outside of direct reinforcement, ala behavioral theory.
- Cognitive theories examine the intersection of how thoughts are connected to beliefs and behavior.
Furthermore, Exposure Therapy, a subset of CBT (approached slightly different in Behavioral Therapy) is based on emotional processing theory (Kaczkurkin and Foa, 2015):
- Emotional Processing theory investigates how fear occurs through networks of association- how it is maintained or broken.
When did CBT first come into use?
As with most things that involve credit giving and fame, the début of most theories can be likened to an academic bare-knuckle brawl which lends to the asserting of various individuals and institutions as the rightful heir to said throne. Yes, the key names in its development were certainly Aaron Beck and Albert Ellis, but just as multiple theories converged to birth CBT, so did multiple researchers, voices, and systems. By and large, cognitive theory, led by Beck, began disrupting the dominant behavioral theories in the 1960’s and 70’s, gaining steam in the therapeutic community by late 70’s and 80’s.
Ride the wave.
CBT is often seen in “three waves (Hayes and Hofmann, 2017).”
- Behavior therapy set the foundation of empirical research and focus on learning.
- Cognitive theories led to focus on maladaptive thinking patterns and their effect. This birthed “classic CBT.”
- More recently, or the “third wave” focuses less on content of thought and more on relationship to behavior, thought, and emotion. This has given way to consideration contextually of the person with applications such as:
- Mindfulness
- Emotions
- Values
- Goals
- Metacognition
What does it treat?
Treatment for Anxiety, Depression, and OCD are common with CBT. You can find the robust treatment of PTSD, substance abuse, relationship problems, eating disorders, Bipolar Disorder, psychosis, chronic pain, general health, and much more, as well.
Any successful treatment has its limits, and Cognitive Behavioral is no different. Autism by and large is treated through Behavioral Therapy (specifically ABA). Those looking for supportive psychotherapy (talk therapy) to verbally process may prefer someone who spend more time working with this approach (though many CBT clinicians are quite good when warranted). Personality disorders are thought to be better treated holistically by DBT, which, though originally based out of CBT, is distinct in some regards. Furthermore, those lacking insight or awareness may not respond well to the requirements of CBT that involves self-monitoring and actively engaging in various changes based on the individual’s awareness and willingness.
Hallmarks of CBT.
- By and large, CBT is present-focused and very solution driven. This does not mean a clinician will not gain past history, or if warranted, address topics or issues in the past. However, CBT therapists will predominantly work in the present to explore how your current thoughts, feelings, and actions (even about past events or future considerations) can address problems or goals while reaching reasonable goals of well-being.
- It is hands-on, typically homework driven, and can incorporate some elements of teaching (psychoeducation).
- It is largely a demystified approach. Providers will often teach the very tools and underpinnings of the therapy process so a client can take them home and implement themselves, ideally decreasing dependence on a clinician.
- It has gotten a reputation at times, especially in the first two waves, as unfeeling and mechanical. It is a common misnomer that some assume the therapeutic relationship is seen as unimportant, or that it is advice-driven. Though some early conceptions may be warranted towards this, it is largely untrue as a whole; it is robust, relational, collaborative, and seeks to establish rapport between therapists and clients.
- By and large, CBT has the most empirical support, though its approach also lends itself at times to empirical research (monitoring and tracking symptoms through scales, for instance, rather than more subjective self-report). This is not to argue empirical is necessarily better, but in empirical literature it comes out with the greatest support (Hofmann et al., 2012).
- Short term- typically brief, it is not uncommon for many problems to be treated in 12 sessions by CBT. However, divergence does occur when highly personalized to an individual, with factors of severity, comorbidity, etc., impacting timeframe.
Personalized hallmarks of CBT.
While CBT is largely characterized by the above, variations exist additionally, such as in my practice, where appropriate:
- Facing fear rather than exclusively seeking only to relieve fear (thereby in many cases offering more durable relief). Exposure therapy is one tool used to accomplish this.
- Involvement of client system and support.
- Incorporation of spiritual beliefs and values.
- CBT is successful in a variety of environments, with its treatment appearing to work very well through telehealth, intensive treatment, home visits, appointments in-vivo, and more.
- Skills are often translatable to other life issues. For example, it is common that a person who learns to restructure unrealistic thoughts in depression can then begin applying in other domains (and hopefully they do!), such as in critical thinking in business, healthy self-talk in parenting, or positive realms such as being realistic with a job bonus or new relationship.
CBT and you.
Though there are many effective therapy treatments to date for a range of issues, CBT comes out as the most researched, most helpful for the widest range of problems, and can be highly personalized. If you are considering (or reconsidering) CBT, it is crucial to advocate for yourself and ask good questions of a potential counseling provider, typically in a first session:
- How much success do you see in treatment?
- When do you refer out to others?
- What is your training and background?
- How much experience do you have treating individuals with______?
- How much of your current practices involves _____?
- What are your views on medication?
I hope you will be assertive and advocate for yourself as a client to gain good treatment. Know that no matter the psychotherapy, it is still based on the therapeutic relationship, which means your best treatment must involve an open, honest, and assertive communication- make sure to say what’s working for you and what’s not! I wish you the best in your journey of mental health, and if indicated, hope that CBT helps make as much of a difference in your life as most of my clients (and in my own life).








Leave a Reply